Revisiting the Rationing of Medical Degrees in the United States
The first time Spencer applied to medical school, he sent applications to 28 colleges across the country. As a well-rounded graduate of an Ivy League university with extensive biomedical research experience, he felt confident that he would get accepted somewhere. When he was unsuccessful, he retook the MCAT, got a higher score, and narrowed his search to a few state schools with high acceptance rates for in-state applicants. Still nothing. By the third time around, Spencer felt resigned to apply out of the country. “I decided to go to the Caribbean. I knew [medical school] was something I was capable of, and I thought I wasn’t given an opportunity,” Spencer explained.
Since 2000, 24 new offshore for-profit medical schools have opened in the Caribbean, with over 20,000 graduates like Spencer currently practicing in the U.S. (Spencer eventually became a general internist). Acceptance to stateside post-graduate residency positions from these schools is only around 50%, though. This means half of the graduates are left to either retry next year or abandon medicine altogether. At the same time, the U.S. is facing a serious shortage of physicians. Revised estimates place the overall deficit anywhere between 61,700 and 94,700 doctors by 2025, especially in primary care, where the projected shortfall ranges between 14,900 and 35,600.
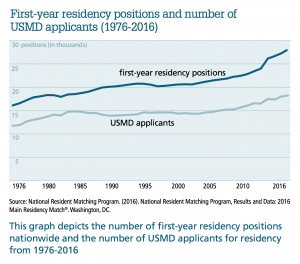
As the country debates how to fix this shortage, one factor that has garnered relatively little attention is why there are so few MDs graduating from U.S. medical schools (USMDs). In 2016, less than two-thirds of residency positions nationwide were filled by USMDs, with nearly 94% of them successfully “matching” to a residency program. In other words, after almost every graduating USMD got a residency position, there were still nearly 11,000 residency spots left over. They would be filled by non-USMDs, specifically osteopathic and international medical graduates. (U.S. osteopathic doctors, or DOs, are trained under a parallel medical curriculum that is nearly identical to MDs’, but with additional emphasis on whole-person care and disease prevention). For the past ten years, there have been between 29-35% more residency positions than U.S. seniors applying for them—an average of 1.47 positions per USMD applicant.
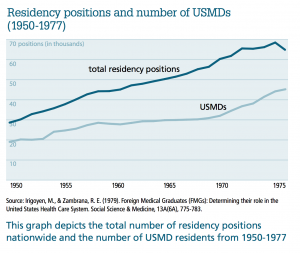
These “extra” positions should not be mistaken for an overabundance of physicians, however, as the nationwide shortage of doctors persists despite the fact that DOs, U.S.-citizen international medical graduates (USIMGs), and non-U.S. citizen international medical graduates (IMGs) respectively fill approximately 8.6%, 10.3%, and 13.5% of residency positions each year. Hospitals, which benefit tremendously from inexpensive resident labor, have pushed Congress to increase the funding allocated to graduate medical education and expand residency programs, with only limited success. Yet despite the impending shortage of doctors, the proportion of USMDs to residency positions has remained relatively unchanged since the early days of modern medical training. Since 1950, the U.S. has consistently graduated anywhere between 20% and 45% fewer USMDs than are needed to fill residency positions nationwide (see page 38).
This gap is not for lack of interest in medical careers; in 2014, for example, only 43% of all medical school applicants in the U.S. were admitted to traditional medical schools, suggesting that far more people are interested in medicine than there are spots available. Although it is costly to open new medical schools or expand existing ones, medical schools in the U.S. have responded to the predicted shortage by increasing enrollment by almost 20%. Even so, the number of USMDs remains far from sufficient to fill all residency positions, despite the profession having had ample opportunity to ramp up its production of doctors since the 1950s. The question is, why?
Degree Rationing Increases USMDs’ status
The answer may have to do with increasing professional status. One of us (Jenkins) spent 23 months from 2011-2014 observing and interviewing USMD and non-USMD residents and hospital administrators at two different Northeastern internal medicine programs, as part of a broader study on the medical profession. The fieldwork revealed status distinctions between USMDs and non-USMDs—even within the same specialty—and sought to identify some of the mechanisms contributing to these distinctions.
One reason USMDs enjoy higher status is because they are relatively scarce. As one American-trained resident noted, USMDs’ exclusivity “makes us something special. Costly and rare.” This phenomenon, known as degree rationing, may or may not be a conscious intention of the profession, but by under-producing doctors, USMDs remain in high demand by residency directors. That demand increases their value and prestige compared to non-USMDs. This is important because thousands of international and osteopathic graduates fill residency positions every year, and by importing what some have described as the “world’s best and brightest,” the U.S. medical profession risks competition from highly skilled non-USMDs.
To help stave off this competition, state licensing boards, staffed primarily by USMDs, require all internationally-trained physicians to complete at least three years of residency before practicing independently in the U.S. Requiring non-USMDs to apply alongside USMDs for residency positions, regardless of their level of previous training, levels the playing field considerably. (A fully trained dermatologist from another country, for example, must apply to redo a dermatology residency alongside USMD senior applicants). Because USMDs are generally considered higher status than non-USMDs, in part due to degree rationing, they more often match to desirable and prestigious specialties. In 2016, for example, nearly 76% of residency positions in surgery were filled by USMDs, even though they comprised only 55% of applicants. In contrast, non-USMDs generally occupy positions in less competitive fields like family medicine, where they comprise nearly 55% of new residents.
Importantly, there are no formal regulations requiring residency programs to prioritize USMDs, so prestige becomes an important, albeit informal, mechanism for ensuring their access to top positions. Programs benefit from USMDs’ high status, too. A hospital administrator explained: “One way that you increase the prestige of the training program is to eliminate international medical grads.” Elite programs therefore attract elite applicants (USMDs), who, in turn, help reinforce the program’s prestige.
Professions have long been described by sociologists as cartels that monopolize the provision of certain services to protect against competition from other occupations. Doctors, for example, have the exclusive permission to perform surgery, a service that makes them highly valuable in society. If physical therapists could also perform surgery, surgeons would likely lose status and income, because patients could go to alternative professionals for the same service. Professions therefore try to delineate “jurisdictions” to keep other professions from competing for their clients—something medicine has been exceptionally good at, despite incursions into its technical core by other professionals, such as nurse practitioners and physicians’ assistants.
An important dimension of this dominance is controlling the supply of doctors. This keeps the value of membership high and enhances the profession’s contention that only a select group of people can do the highly technical work that distinguishes the profession from its competitors (a process known as “external social closure”). Our findings, however, suggest that scarcity may also be useful for internal social closure—staving off competition from the inside. As the number of international and osteopathic graduates vying for residency positions increases every year, American MDs must remain valuable—and scarce enough—to successfully fend off the additional competition. This is especially true if hospitals prefer recruiting top-notch international or osteopathic graduates who may have better test scores or interpersonal skills than “bottom of the barrel” USMDs. Match statistics reveal that, in specialties like internal medicine, IMGs have to score up to three standard deviations higher on their licensing exams to have the same probability of matching to residency as USMDs, which suggests that the elite core of the profession has been remarkably successful at protecting its insiders, despite fierce competition from those trained outside the usual channels.
A History of Titrating Supply
Importantly, the U.S. has a long history of using top-down approaches to control the nation’s supply of doctors. Since the beginning of modern residency training, the country has relied particularly on IMGs, whose influx has been regulated through centralized governmental policies such as visa restrictions and licensing laws. Depending on the perceived supply of USMDs at any given moment, policies have either increased or decreased the number of IMGs allowed into the U.S. to practice medicine, with the aim of protecting the elite USMD core of the medical profession.
The Smith-Mundt Act of 1948 extended exchange visitor (J) visas to IMGs for the first time, allowing them to pursue residency training in the U.S. on the condition that they leave the country for at least two years prior to applying for permanent residency. This meant, however, that while the U.S. was attracting more foreign doctors, those doctors were not staying in the country after their training, thereby doing little in the long-term to add to the nation’s medical workforce.
By the early 1960s, the Department of Labor determined that a doctor shortage was looming, so laws were passed to facilitate an influx of IMGs. In 1961, the Mutual Educational and Cultural Exchange Act (also known as the Fulbright-Hays Act) waived the two-year foreign residency requirement for IMGs. By 1962, doctors were exempted from national quotas that limited the number of migrants from certain countries. Preference categories for skilled workers were created in the 1965 Immigration Act, encouraging the immigration of professionals who could help fill gaps in the U.S. economy. And by 1970, IMGs could simply exchange their J-visas for regular work (H-1B) visas to facilitate their application for permanent residency. Unsurprisingly, the supply of IMGs increased considerably.
Concerns about the shortage of doctors were replaced with fears of an oversupply from the 1970s until the 1990s. These fears stemmed from a perceived abundance of international medical graduates. Around this time, offshore medical schools began emerging in the Caribbean, offering an outlet for U.S. citizens wanting to become doctors but unable to gain entry to mainland universities. Numbers were also rising domestically: between 1965 and 1985, the number of U.S. medical schools increased from 88 to 127, with an increase in the total number of yearly graduates from 7,574 to 16,191. Ten new osteopathic schools opened in the US between 1968 and 1988, further crowding the workforce.
The result was an estimated surplus of doctors ranging anywhere between 35,000 to 70,000 doctors. Panic ensued. Scholars wrote about the threat of unemployment for junior doctors and how the outlook was grim for USMDs applying to residency. The government passed the Health Professions Educational Assistance Act of 1976 and the Health Services Extension Act of 1977, which reinstated the two-year foreign residency requirement for J-visa holders and required new IMGs to apply to the Department of Labor for approval of their visa. In the mid-1990s, the American Medical Association, the Pew Health Professions Committee, the Institute of Medicine, and other professional bodies called for the contraction of residency positions and a reduction in the number of IMGs to protect USMDs from the impending physician surplus. Based on policy directions from the late 1970s to the mid-1990s, many expected the nation to become less dependent on IMGs, eventually preferring to hire American-trained personnel over foreign doctors.
Yet, self-sufficiency has not come to pass. The country remains as dependent on non-USMDs as in the 1950s and ‘60s. Even the laws have relaxed again to allow non-U.S. citizens to practice and ultimately stay in the country long-term. (Depending on the residency program, IMGs can be sponsored for either H1-B or J-visas, with the option of waiving the two-year home residency requirement by working in an underserved area upon graduation.) Why not simply graduate enough USMDs so that the country no longer has to rely on international and osteopathic doctors, thereby eliminating competition altogether? After all, Medicare pays for residency training—yet another reason to invest in American talent.
The Social Contract
Findings suggest that this gap persists to buffer USMDs from having to take residency positions in less attractive locations, specialties, or hospitals, relying instead on non-USMDs to fill these spots. As long as doctors are in sufficiently high demand, there is little incentive for USMDs to dramatically increase their supply; non-USMDs fill the positions that few want to fill. As one medical school administrator put it, “The whole system is set up to basically reward [USMD] students.” Self-sufficiency could therefore threaten the livelihoods that American medical students have come to expect.
Many USMDs undergo medical training with the understanding that in exchange for hard work, debt, and deferred gratification, they will be able to pursue the career of their choice in the specialty of their choosing—representing a kind of social contract between trainees and the profession. As one USMD resident described: “There are a lot of people that want to go into this field [medicine] and not everyone is going to make it, so the ones that are able to make it [into a US medical school]—I’m going to sound very awful—but I think we deserve something. …I feel like, if I can get to that next step, I should be entitled to the things that come along with that,” referring to getting priority for top residency spots. In the words of another USMD resident, “It’s maybe fair for U.S. medical students to be prioritized [for] U.S. residency positions… we’re kind of paying our dues to get these spots, in some sense.” Indeed, as sociologists Caroline Hodges Persell and Peter W. Cookson have found, going to an elite school is often associated with a perceived set of “rights” or guarantees—in this case, admission to their preferred residency.
Other USMD residents described the contract more explicitly as a return on their investment: “I think you have to accommodate the people that have put money into their education here before you train outside physicians to do the job.” Another USMD intern said pragmatically, “I’m $130,000 in debt, right? I’m not willing to put that on a degree that I don’t know is going to get me a job afterwards.” Thus, U.S. medical trainees go through schooling with the expectation that their considerable investment of time, money, and effort will be rewarded with lucrative positions in favored specialties and locations. If the U.S. achieved self-sufficiency in terms of staffing its residency programs, USMDs would undoubtedly have to fill positions in undesirable geographic and professional areas, and potentially embark upon careers they did not sign up for—or worse, be left with no medical career at all.
The legal profession provides a powerful cautionary tale in this regard. The Great Recession of 2008 prompted many individuals to turn to law school as a “safe” route toward near-guaranteed employment. It resulted in a massive surplus of lawyers. Today, lawyers are facing unemployment, layoffs, and significant student debt, in part because the relative demand for lawyers is closely linked to the vagaries of financial markets. (Demand for doctors, in contrast, is far more stable and relatively impervious to market forces, so the rationing of supply leads to more predictable outcomes.) As the markets struggle to bounce back, the legal profession can no longer guarantee that it can fulfill law students’ expectations of gainful employment and a degree of social prestige. As you might expect, interest in the profession has declined. In 2015, only 41,000 individuals applied to law school nationwide, compared to 90,000 in 2004 and 77,000 in 2010. Getting a job as a lawyer is no longer a sure thing, and as a result, law schools have been described as being in a “death spiral,” with some schools laying off faculty due to decreased enrollment.This is precisely the kind of situation that medicine has managed to avoid by ensuring that the number of USMDs is lower than the number of training positions available. The current social contract in medicine hinges on being able to offer U.S. medical students gainful and satisfying employment upon graduation. As one USMD resident explained, “With the number of spots, anyone can get into law school, but not everybody can get a job. But we can. We have good job security.” Should the terms of the contract change, however, fewer medical graduates may want to enter a profession that does not guarantee job security or fulfillment of aspirations, an outcome that would undoubtedly worsen the current shortage of physicians.
Questions Remain
As the country struggles to address a nationwide shortage of doctors, we should not overlook the profession’s inner dynamics. In addition to helping professions control the service market (a longstanding contention of the literature on social closure), we find that rationing may also help professionals control competition in a globalizing market for medical education.
These results leave us perhaps with more questions than answers. What are the material and symbolic barriers to increasing the supply of USMDs? How would self-sufficiency in residency positions impact the profession’s social contract with its trainees? Should USMDs get priority above all other candidates for residency positions? Should fully trained IMGs be required to redo residency? And what are the impacts of rationing on doctors’ well-being and burnout, given that there are fewer doctors to address demand? To address the physician shortage, policymakers will have to consider how the profession’s social contract with its own ranks may be perpetuating an underproduction of doctors.
Recommended Readings
IHS Inc. 2016. The Complexities of Physician Supply and Demand 2016 Update: Projections from 2014 to 2025. Washington, DC: Prepared for the Association of American Medical Colleges. A look at current projections of supply and demand within medicine for the next ten years.
David Grusky. 2011. “Occupy the Future: Rationing Education Protects the Rich,” Boston Review. An account of degree rationing in elite institutions by a leading sociologist of stratification.
Matilde Irigoyen and Ruth E. Zambrana. 1979. ”Foreign Medical Graduates (FMGs): Determining their role in the United States Health Care System,” Social Science & Medicine 13A(6A):775-783. A historical look at how the U.S. has controlled the external influx of doctors.
National Resident Matching Program. 2016. National Resident Matching Program, Results and Data: 2016 Main Residency Match®. Washington, DC. A yearly report on the Residency Match results, including information about the placement of USMDs and non-USMDs.
Caroline Hodges Persell and Peter W. Cookson, Jr. 1985. “Chartering and Bartering: Elite Education and Social Reproduction,” Social Problems 33(2):114-29. A classic article about the special “status rights” that accompany an elite education.